Team:Lethbridge/project
From 2014.igem.org
| Line 37: | Line 37: | ||
[[Image:Exosome_Logo.jpg|100px]] | [[Image:Exosome_Logo.jpg|100px]] | ||
| + | |||
| + | <h2>Background & Rationale</h2> | ||
| + | |||
| + | <p>Astrocytes are abundant forms of glial cells located in the brain and spinal cord that serve to regulate cerebral blood flow and synapse function [1]. Central nervous system (CNS) injuries and neurodegenerative diseases are frequently accompanied by reactive astrogliosis, a process whereby astrocytes isolate damaged neural tissue, restrict inflammation, stimulate blood-brain barrier repair, and reduce further degeneration of surrounding brain tissue [2]. However, the formation of this obstructive “glial scar” also impedes future neural regeneration and axon remyelination and thus is a significant obstacle to rehabilitation in the CNS [3].</p> | ||
| + | |||
| + | <p>Interestingly, a recent study demonstrated the direct reprogramming of in vivo murine and cultured human reactive astrocytes to functional neurons using the retroviral expression of a single transcription factor, NeuroD1 [4]. Thus, NeuroD1 (if appropriately targeted to reactive astrocytes in damaged CNS tissue) has the potential to significantly improve current neural regeneration therapies. However, direct application of NeuroD1 to the human brain would not only be largely non-specific (and require the use of controversial viral delivery systems) but also excessively invasive. Consequently, the development of novel therapeutic delivery mechanisms is necessary to specifically target DNA, RNA, proteins, and other biologically relevant molecules to damaged or diseased neural cells. Microglia, another class of glial cell prevalent in the CNS, migrate to regions of neural damage and are the primary immune response in the CNS [5]. Their mobility, proximity to reactive astrocytes (and thus neural damage), and exosomal communication make them suitable candidates as potential delivery mechanisms for CNS injury-related rehabilitative therapies [6].</p> | ||
| + | |||
| + | <h2>Objectives</h2> | ||
| + | |||
| + | <p>Altogether, the aim of this study is to harness microglia as non-immunogenic carriers of neural tissue-specific therapeutic genes. Specifically, in an effort to promote functional recovery after CNS insult, these microglial cells will express a synthetic plasmid delivery system that exploits endogenous exosome production capabilities to deliver a neural reprogramming message. Our specific objectives include:</p> | ||
| + | |||
| + | <p>1) Generate microglial cells that package plasmids into exosomes and secrete them at regions of neural damage.</p> | ||
| + | |||
| + | <p>2) Use these engineered microglia to target stable plasmid DNA copies of the reprogramming factor gene NeuroD1 to regions of astrogliosis in a cell culture model of Traumatic Brain Injury. NeuroD1 will be selectively expressed in reactive astrocytes, thereby directly converting obstructive glial scars to neurons (replacing at least some of those lost to damage or disease) and reducing the inhibitory environment produced by the reactive astrocytes.</p> | ||
| + | |||
| + | <p>3) Design a novel antibiotic-free plasmid selection system that will allow generation of the NeuroD1-carrying plasmids while avoiding the introduction of antibiotic-resistance coding genes into human cells. Our proposed system will also minimize the size of our plasmid for ease of exosomal packaging.</p> | ||
Revision as of 01:46, 17 October 2014

Project
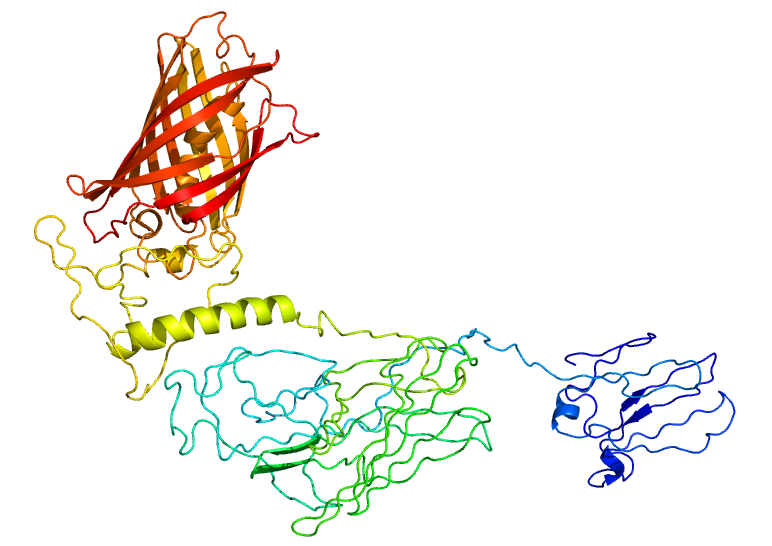
Figure 1. Confocal Image of HEK cells transfected with Lamp2B-clover construct. Description goes here.
Figure 2. Confocal Image of HEK cells transfected with Lamp2B-clover construct. Description goes here.
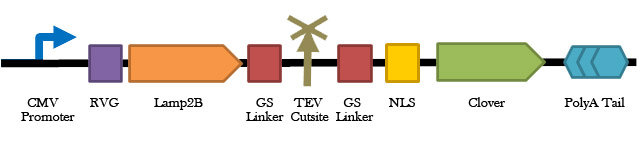
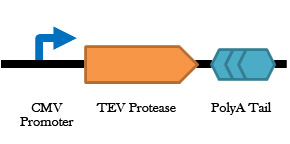
Figure 3. Construct design for the TEV protease. Description goes here.
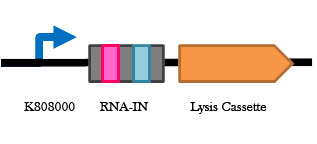
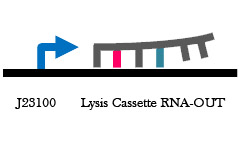
Figure 4. RNA-IN/OUT construct design. Description goes here.
Background & Rationale
Astrocytes are abundant forms of glial cells located in the brain and spinal cord that serve to regulate cerebral blood flow and synapse function [1]. Central nervous system (CNS) injuries and neurodegenerative diseases are frequently accompanied by reactive astrogliosis, a process whereby astrocytes isolate damaged neural tissue, restrict inflammation, stimulate blood-brain barrier repair, and reduce further degeneration of surrounding brain tissue [2]. However, the formation of this obstructive “glial scar” also impedes future neural regeneration and axon remyelination and thus is a significant obstacle to rehabilitation in the CNS [3].
Interestingly, a recent study demonstrated the direct reprogramming of in vivo murine and cultured human reactive astrocytes to functional neurons using the retroviral expression of a single transcription factor, NeuroD1 [4]. Thus, NeuroD1 (if appropriately targeted to reactive astrocytes in damaged CNS tissue) has the potential to significantly improve current neural regeneration therapies. However, direct application of NeuroD1 to the human brain would not only be largely non-specific (and require the use of controversial viral delivery systems) but also excessively invasive. Consequently, the development of novel therapeutic delivery mechanisms is necessary to specifically target DNA, RNA, proteins, and other biologically relevant molecules to damaged or diseased neural cells. Microglia, another class of glial cell prevalent in the CNS, migrate to regions of neural damage and are the primary immune response in the CNS [5]. Their mobility, proximity to reactive astrocytes (and thus neural damage), and exosomal communication make them suitable candidates as potential delivery mechanisms for CNS injury-related rehabilitative therapies [6].
Objectives
Altogether, the aim of this study is to harness microglia as non-immunogenic carriers of neural tissue-specific therapeutic genes. Specifically, in an effort to promote functional recovery after CNS insult, these microglial cells will express a synthetic plasmid delivery system that exploits endogenous exosome production capabilities to deliver a neural reprogramming message. Our specific objectives include:
1) Generate microglial cells that package plasmids into exosomes and secrete them at regions of neural damage.
2) Use these engineered microglia to target stable plasmid DNA copies of the reprogramming factor gene NeuroD1 to regions of astrogliosis in a cell culture model of Traumatic Brain Injury. NeuroD1 will be selectively expressed in reactive astrocytes, thereby directly converting obstructive glial scars to neurons (replacing at least some of those lost to damage or disease) and reducing the inhibitory environment produced by the reactive astrocytes.
3) Design a novel antibiotic-free plasmid selection system that will allow generation of the NeuroD1-carrying plasmids while avoiding the introduction of antibiotic-resistance coding genes into human cells. Our proposed system will also minimize the size of our plasmid for ease of exosomal packaging.
 "
"